Noise is one of the most persistent challenges in healthcare environments. Constant alarms, conversations, and equipment sounds can easily exceed recommended nighttime noise levels of 35–40 dB(A), leading to sleep deprivation, stress, and slower recovery.
Noise is one of the most persistent challenges in healthcare environments. Constant alarms, conversations, and equipment sounds can easily exceed recommended nighttime noise levels of 35–40 dB(A), leading to sleep deprivation, stress, and slower recovery.
A 2025 Mayo Clinic study, published in Sleep Medicine: X, provides compelling evidence that sound masking systems—especially those using white noise—significantly improve sleep quality and patient comfort in hospitals.
Clinical Findings: White Noise Enhances Sleep Efficiency
In their systematic review of 1,920 studies, Mayo Clinic researchers identified seven randomized controlled trials involving nearly 500 hospitalized adults. Across these studies, white noise or similar masking sounds consistently led to measurable improvements in sleep efficiency, total sleep time, and perceived restfulness.
For instance, one coronary care unit trial showed that sleep quality scores more than doubled after three nights of white noise exposure. Another reported significantly higher sleep efficiency and duration (p < 0.003). Importantly, fewer than 2% of participants reported discomfort, confirming the safety and tolerability of masking sounds in clinical settings.
As the authors note, “White-noise and other similar masking noises seem to improve sleep efficiency in hospitalized adults, with good tolerability.”
Khandelwal et al., Mayo Clinic, 2025

Why Acoustic Control Matters for Patient Recovery
The connection between acoustics and patient health is now well-established. Poor sleep quality is linked to longer recovery times, weakened immune response, and increased risk of delirium, particularly among older patients.
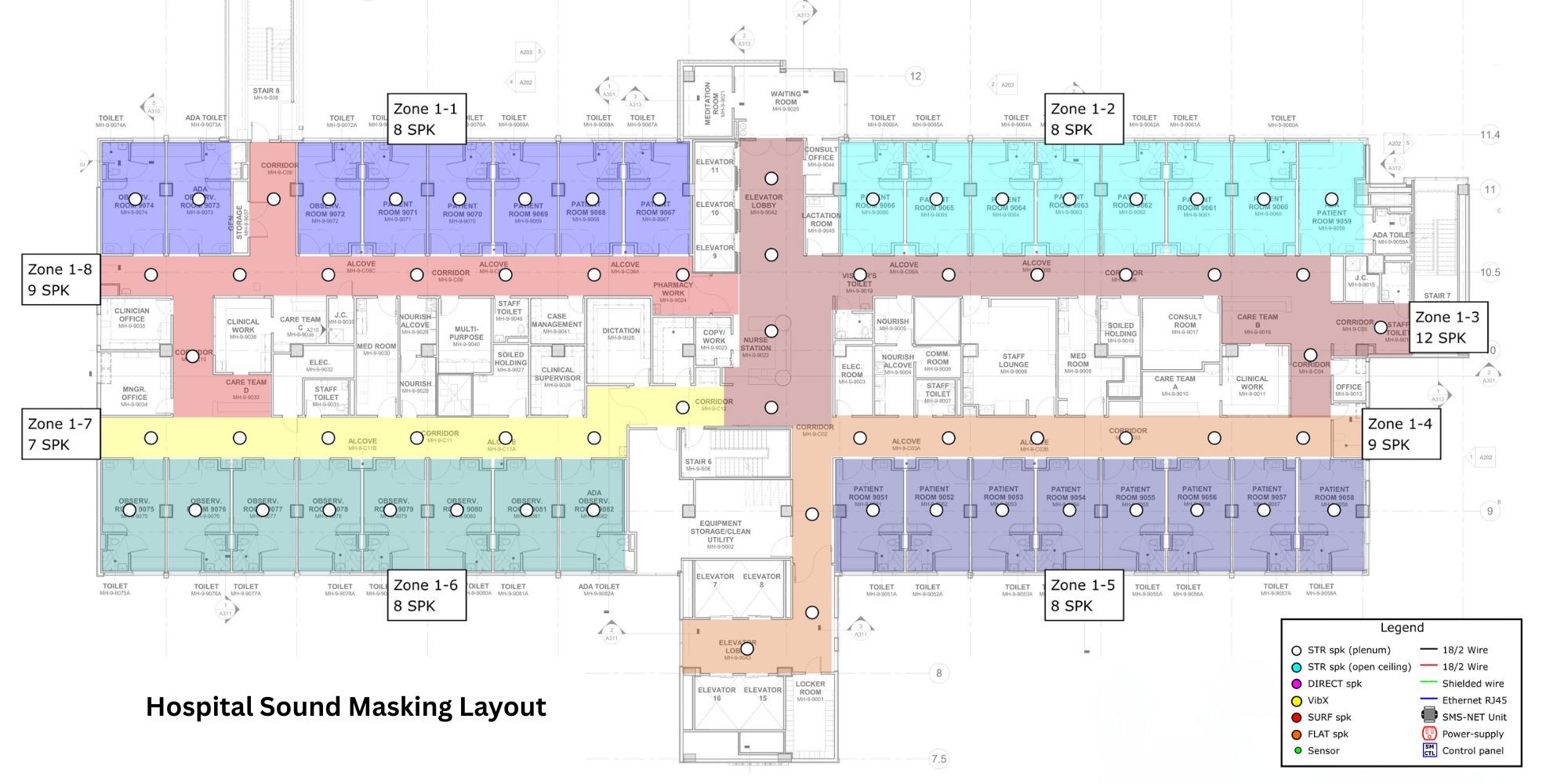
Sound masking systems introduce a neutral, consistent acoustic layer that reduces the perception of sudden noises such as alarms, footsteps, or conversations. This creates a more stable sound environment that promotes rest and lowers physiological stress.
Supporting studies further validate these benefits:
- Xie, Kang & Mills (2009) concluded that “sound masking appears to be the most effective technique for improving sleep in intensive care units.” Source
- The CISCA Acoustics in Healthcare Guide recommends “specifying sound-masking systems in patient rooms to reduce interruptions from equipment alarms and signals.” “Specify ceiling-housed, sound-masking systems in open areas (e.g., waiting rooms) that cover the speech frequency range at the lowest volume, as architectural elements that typically block sound (e.g., walls) are minimal in these spaces.”
Beyond Sleep: The Broader Health Benefits of Sound Masking
While the Mayo Clinic study focuses on hospitals, other research highlights broader well-being effects. A 2023 study from Eindhoven University found that adaptive sound masking in workplaces reduced stress, tension, and fatigue, helping participants feel calmer and more focused.
Bergefurt et al., 2023
Health Canada also confirms the safety of sound masking levels, stating that “there is no known risk of hearing loss associated with sound levels below 70 dBA.” Given that sound masking systems typically operate around 40 dB(A), they are far below any risk threshold.
Health Canada, 2023
Toward Healthier, Quieter Hospitals
The Mayo Clinic’s research reinforces a growing consensus: sound masking is an evidence-based, non-pharmacological solution for better patient rest and recovery. From intensive care units to patient suites, integrating acoustic control helps hospitals create calmer, more restorative environments.
Soft dB’s healthcare sound masking systems are scientifically engineered to deliver this balance—reducing disruptive noise, enhancing sleep quality, and supporting patient well-being.
As hospitals evolve toward more patient-centered design, sound masking isn’t just a comfort feature—it’s a clinical advantage.